Calcium
Calcium (Ca2+) is a prevalent element in the body, and comprises about 1.2 Kg of our weight. Although 99% of this Ca2+ is found in bones, the small amount of Ca2+ found in the extracellular fluid is critically important. Ca2+ is an important physiologic mediator, and participates in muscle contraction, neuronal function, and regulation of enzymatic processes. It is critical to maintain constant levels of plasma Ca2+, and thus a number of physiological mechanisms participate in this regulatory process.
In previous courses, you have learned about the renal and endocrine mechanisms that regulate blood Ca2+ levels. A number of pathophysiological conditions can lead to elevated blood calcium (hypercalcemia) or reduced blood calcium (hypocalcemia). This module focuses on the effects of hypercalcemia and hypocalcemia on neuronal excitability and neuromuscular activity.
Since Ca2+ entry into a nerve terminal causes neurotransmitter release, you might think that hypercalcemia would result in exaggerated neurotransmitter release and neuronal hyperactivity. In contrast, the effects are the opposite.
High Ca2+ levels (hypercalcemia) can block sodium movement through voltage-gated sodium channels, causing reduced depolarization and impaired action potential generation. This explains the fatigue, cognitive impairments, muscle weakness, low muscle tone, and sluggish reflexes in muscle groups during hypercalcemia. Severe hypercalcemia is considered a medical emergency: coma and cardiac arrest can result due to the effects of Ca2+ on sodium entry into cardiac myocytes and neurons.
In contrast, low Ca2+ levels (hypocalcemia) facilitate sodium transport, as the normal inhibition by Ca2+ of sodium movement through voltage-gated sodium channels is lost. Thus, low Ca2+ levels result in hyper-excitability of excitable cells, such as neurons. At plasma Ca2+ ion concentrations about 50 percent below normal, the peripheral nerve fibers become so excitable that they begin to discharge spontaneously, initiating trains of nerve impulses that pass to the peripheral skeletal muscles to elicit tetanic muscle contraction.
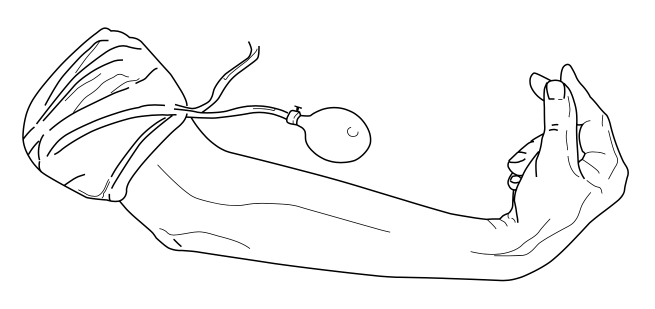
A diagnostic indicator of hypocalcemia is Trousseau's sign. Trousseau's sign presents as carpopedal spasms following inflation of a sphygmomanometer cuff above systolic blood pressure. Occlusion of the brachial artery causes flexion of the wrist and metacarpophalangeal joints, hyper-extension of the fingers, and flexion of the thumb on the palm, producing a characteristic posture. The proposed mechanism for Trousseau's sign is increased excitability of the nerves in the arm and forearm by hypocalcemia, such that the nerves fire when subjected to ischemia after inflating the cuff.
Another indicator of hypocalcemia is Chvostek's sign, which is elicited by tapping the cheek over the path of the facial nerve. In hypocalcemia patients, the facial muscles on the same side of the face will contract momentarily, as the tap will stimulate hyperexcitable motor axons.
A rarer consequence of hypocalcemia is seizures.
The table below summarizes the typical effects of hypercalcemia and hypocalcemia on excitable membranes.
| Condition | Characteristics |
|---|---|
| Hypercalcemia | Fatigue, cognitive impairments, muscle weakness, low muscle tone, sluggish reflexes |
| Hypocalcemia | Tetany, Trousseau's sign, Chvostek's sign |
This movie provides more insights into the effects of hypercalcemia and hypocalcemia on excitable membranes.
If the movie does not play in this window, or you would like to see it in a window of alternate size, download it from this link.
Magnesium
Another ion that can affect neuronal and muscle excitability is magnesium. Plasma magnesium levels are affected by changes in gastrointestinal and renal absorption of the ion, as well as a number of metabolic disorders you will discuss in subsequent courses. High levels of magnesium (hypermagnesemia) block Ca2+ movement through voltage-gated Ca2+ channels, particularly those of the peripheral nervous system, such as terminals of motoneurons and sympathetic and parasympathetic nervous system neurons. As a consequence, neurotransmission at these terminals is reduced, resulting in slowed muscle contraction, decreased or absent muscle reflexes, impaired breathing (due to decreased neurotransmission at the diaphragm), and lowered blood pressure (due to effects on the sympathetic nervous system).
If magnesium levels are too low (hypomagnesemia), the normal inhibition of Ca2+ movement through voltage-gated Ca2+ channels dissipates, so neurotransmission increases. This is particularly prominent at the neuromuscular junction, resulting in tetany and muscle spasms.
This movie provides more insights into the effects of hypermagnesemia and hypomagnesemia on excitable membranes.
If the movie does not play in this window, or you would like to see it in a window of alternate size, download it from this link.